 |
|
Fisher et al published the first attempt at engineering a full-scale adult human femur head from hMSCs. This is the largest reported tissue to have been engineered and took over 700 million hMSCs to fabricate.
|
John Fisher’s laboratory at the University of Maryland, College Park recently published what can be considered a significant advance for Tissue Engineering and Regenerative Medicine. Graduate student Bao Nguyen and her colleagues have engineered a bone construct that is 20 times larger than any reported previously, and the size of an adult human femur.
Why is this important? Critical size bone defects are a significant health problem (resulting in over $1 billion in annual healthcare costs incurred in the U.S.) and are currently treated with grafts, decellularized bone, or synthetic bone grafts, with sometimes unsuccessful results. As such, modern medicine has been looking to tissue-engineered bone grafts as future treatments for such defects. Human bone marrow-derived Mesenchymal Stem Cells (hBM-MSCs) are a promising cell source for such applications because they efficiently differentiate down the osteogenic path and also secrete paracrine factors that may aid survival and vascularization of engineered bone. Prior to this publication, engineered constructs have been relatively small due to cell and culture limits. One major challenge has been growing hBM-MSCs, while maintaining their function, to sufficient numbers needed for an adult human-sized construct; a challenge addressed by RoosterBio. In addition, nutrient and O2 transfer are often insufficient to maintain cell viability and function throughout larger constructs, especially those of the adult human dimension.
To address this cell culture limitation, the Fisher laboratory developed a Tubular Perfusion System (TPS) bioreactor where cells and scaffolds are cultured in a cylindrical chamber and subject to circular media flow. This system has high nutrient and O2 transfer and efficient waste removal and has been previously used to produce smaller engineered bone and cartilage constructs (See here and here).
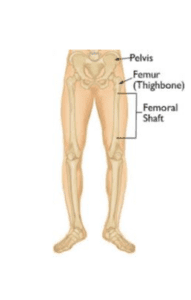
In one study, the authors had access to and combined, for the first time, advanced technologies required for biofabrication: 3D printing, the TPS bioreactor, and scalable production of hBM-MSCs. The goal of the study was to scale-up bone constructs to adult human size. A full-size mold of the superior portion of a human femur (the largest bone in the human body) was 3D printed using information from an opensource database. The mold measured 23 cm long and 10 cm at its widest point with a volume of 200 cm3. The mold was filled with hBM-MSCs in alginate beads (3 mm beads, 100,000 cells per bead). The entire construct utilized 7200 aliginate beads containing a total of 7.2 x 108 cells (yes, that is 720 million cells!). The high volume hBM-MSC cell and media systems used were from RoosterBio, and technical support for the efficient production of large volumes of hBM-MSCs was provided by our company.
After 8 days of culture in the TPS, the construct was examined for cell viability and bone differentiation. High cell viability was seen in all parts of the construct, both on the outside and the inside (interior). In addition, hBM-MSCs committed to the osteogenic lineage throughout the construct, demonstrating the efficiency of the TPS culture system. Both early (Alkaline Phosphotase, ALP) and late (Bone Morphogenic Protein-2, BMP-2) markers of osteogenesis were upregulated relative to day 0. Interestingly, ALP and BMP-2 expression were 25- to 30-fold higher in the construct shaft relative to other portions of the construct. The authors speculate that this is due to shear stress exerted on the parts of the construct closest to the inlet, which activates hBM-MSC signaling pathways, causing the release of paracrine factors that stimulate osteogenesis of the “downstream” shaft portion. Taken together, these results demonstrate that the confluence of cutting-edge technologies such as 3D printing, TPS bioreactors, and best-in-class hBM-MSC manufacturing processes enable the engineering of adult human-sized tissue constructs.
While “…this first foray into full-scale bone engineering provides the foundation for future clinical applications of bioengineered bone grafts…” the authors point out some limitations to this study. The 8 day culture period was relatively short, given the weeks usually needed for high-efficiency bone differentiation. Thus, extended time points and the fabrication of additional large constructs are needed to fully explore the capabilities of the TPS system. Further, alginate is a soft material, and its mechanical properties do not render it the best suited for bone differentiation. In addition, hBM-MSCs within aliginate beads lack cell: cell contact, which may also limit their osteogenic differentiation. To address these limitations of the current system, the Fisher group is developing a 3D printed shell made of an implantable rigid material better suited for the engineering of bone constructs. Finally, the construct lacks a vascular network, which can be overcome by including endothelial cells (EC) in addition to hBM-MSCs or by incorporating micro-channels in the engineered constructs through a variety of methods (e.g. biomaterial fabrication and 3D printing). Despite the aforementioned limitations, the work presented is a significant advance towards clinical-sized tissue-engineered bone constructs for use in patients.
In an attempt to elicit discussion, I will mention other methods that harbor the potential for use in such large-scale tissue engineering applications. For one, hBM-MSC aggregates could be used in place of cells in alginate beads. These 3D-MSC not only maintain cell: cell contact but also undergo osteogenic differentiation more efficiently than cells grown on tissue culture plastic, are resistant to hypoxia, and secrete angiogenic cytokines. Secondly, factors that stimulate bone differentiation of hBM-MSCs, and/or alter mechanical properties of the construct, could be incorporated into the polymer scaffolding or could be introduced into 3D-MSC aggregates. Finally, once bio-inks are developed further, the bone construct could be patterned by 3D printing of cells (hBM-MSC, EC, 3D-MSC) and materials. Now that human-sized constructs are possible in terms of cell numbers and O2and nutrient diffusion, the possibilities are virtually endless.
Finally, we sincerely thank Bao Nguyen and John Fisher for being early adopters of RoosterBio hBM-MSCs and joining us in accelerating Regenerative Medicine!
References
Nguyen BB, Ko H, Moriarty RA, Etheridge JM, Fisher JP. Dynamic Bioreactor Culture of High Volume Engineered Bone Tissue. Tissue Engineering Part A. Volume 22, Numbers 3 and 4, 2016, ahead of print. doi:10.1089/ten.tea.2015.0395. http://online.liebertpub.com/doi/abs/10.1089/ten.tea.2015.0395
Disclaimer: I’m sorry that this is paywalled!
Yeatts, A.B., and Fisher, J.P. Tubular perfusion system for the long-term dynamic culture of human mesenchymal stem cells. Tissue Eng Part C 17, 337, 2011.
http://online.liebertpub.com/doi/abs/10.1089/ten.tec.2011.0263
Yeatts, A.B., Choquette, D.T., and Fisher, J.P. Bioreactors to influence stem cell fate: augmentation of mesenchymal stem cell signaling pathways via dynamic culture systems. Biochim Biophys Acta 1830, 2470, 2013.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3461086/
Ma, X et al. Deterministically patterned biomimetic human iPSC-derived hepatic model via rapid 3D bioprinting PNAS, Early Edition doi: 10.1073/pnas.1524510113 http://www.pnas.org/content/early/2016/02/04/1524510113
