Listen to this Blog:
In the Beginning
To understand how biology relates to regenerative medicine, it’s sometimes useful to grasp a broader concept and its “ontogeny.” Even if not useful, perhaps there’s value in rekindling your sense of wonder from time to time? Here, I’m compelled to take you all the way back to around 2.5-Billion Years, B.C. The story begins much like it carries on today: cells gathering energy sources to sustain themselves. They learned to cooperate amidst fierce competition for scarce energy resources in a niche…and thereby prospered. (For this first part, I need to warn you—some minor “embellishment” is here for the sake of a story that is wanting of precise details.)
Before two billion years ago, cyanobacteria emerged with a special talent: conversion of carbon dioxide and water into oxygen via the radiant energy of our young sun. They got so good at this, that—in a relatively short window of time (geologically speaking)—Earth’s atmosphere accumulated a vast quantity of oxygen. Oxygen being reactive and somewhat poisonous to life in those years, the biosphere was forced to evolve means to protect itself. Not only did more advanced mechanisms of DNA repair evolve to defend against that nasty influx of reactive oxygen species (ROS)-induced mutations, but some organisms began to package the genetic biofunctions within new compartments—establishing a division of labor more distant from the “messy” food-processing and metabolic ones. This was very beneficial for those proto-eukaryotic, archaebacteria-like critters, but they were not yet finished evolving into yeasts, placozoans, chordates, primates, and us.
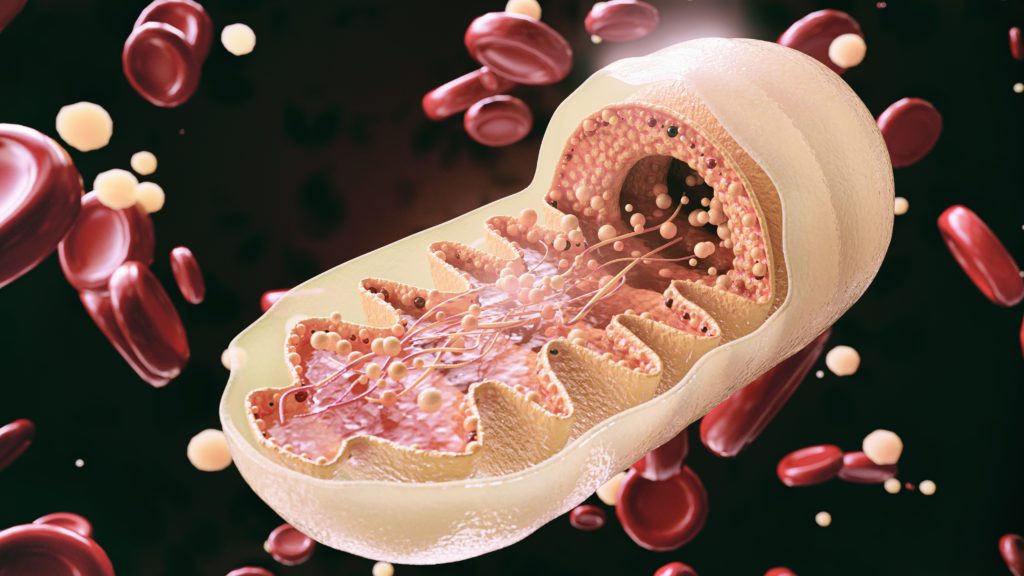
One day, these grandmothers of the eukaryotes encountered fierce “barbarian” cells (i.e., purple non-sulfur bacteria) who sought to invade their neighbors’ cytoplasm and drain them dry of nutrients. Or, perhaps it was the opposite: the proto-eukaryotic scavengers were “hungry” and sought to engulf, to swallow and to digest these smaller, purple prokaryotes. Either way, what was once an adversarial relationship between the two species turned cooperative over millions of years.[1] The purple bacteria and their host cells became “BEFs” – Best Endosymbionts Forever! Gradually, the engulfed bacteria learned to convert the “toxic” oxygen into a high-performance energy currency that these first eukaryotes could use. These two intermingled species even swapped genes, and evolved means of subtle, two-way molecular communication. Behold, the birth of mitochondria—not separate cells but “almost” fully domesticated organelles. Yet, mitochondria never fully abandoned their intercellular defenses—protein toxins that uncannily resemble colicins in shape, though no longer share outward sequence homology, per se.[2] (Perhaps, these early “mitos” donated such related ancestral encoded genes to the nucleus, or sent them far and wide in the phyla via phages?) Colicin-like molecules were once used to poison competitor bacteria by poking holes in their protective outer membrane bubbles. What use were they now? Why not just “disarm” them? Surely, the mitochondria weren’t instructed to “Don’t just DO something; STAND THERE!?” Perhaps, these vestigial toxins were gradually morphed into a rheostatic system to sense stress in their host cells…? That is, when “times got tough,” maybe proto-mitochondria could kill their host and burst out in search of a new, nearby cytoplasm to thrive in. More on that later.
With greater oxygen levels, multicellular life, cell specialization, and organism body plans became possible, all because of that unique partnership between eukaryotic cells and their precious mitochondria.[3] However, the colicin-like reserve arsenal was not forgotten, only repurposed. As vestiges of today’s Bcl-2 family proteins, they became instrumental in programmed cell death, or apoptosis. Cell death that is orchestrated in a tidy fashion is essential to all animal life, including us—for development out of a fertilized egg, or for the mundane removal and recycling of cell materials damaged by mutation, age, or infection. For example, if our own neutrophils did not correctly undergo apoptosis, we’d instantly die from shock due to the release of toxic contents. It seems that mitochondria are not merely responsible for giving us energy. Like the “canary in the coal mine,” the mitochondrion helps sense when a cell and/or her environment is unwell.[4, 5, 6, 7, 8] Further, when she sings her last “note” via depolarization of the electron transport chain, this is a clear signal for the surrounding cell to end its own life for the sake of the whole organism. Our story does not end there, however. We’re beginning to discover still more chapters in the story of mitochondria and multicellular life.
Hey MSCs, Can You Please Spare Some Extra Mito?
Fast forward 1-2 billion years after the first unicellular eukaryotes. Human beings are now running around as infinitely complex biological circuits that wire together not just nuclei, cytoplasm, and mitochondria—but also 30 trillion cells or so. (Fun fact: if the DNA content of each of those cells could be joined end-to-end, they would extend about 10x the distance to Pluto.) Yet it gets even more complex than that. Who would have guessed that mitochondria can and do exchange one cellular residence for another?
Mitochondrial “eviction” obviously occurs in the case of sudden, pathogenic cell lysis as by injury or pathogen. The bacteria-like molecular patterns displayed on free-floating mitochondria convey urgent “damage” signals toward the innate immune system and inflammation,[9] enabling pathogen clearance and later wound healing. What’s more surprising, however, are observations first made by Rustom et al in 2004: cells can form “tunneling nanotubes” between them to connect their cytoplasms, and facilitate organelle transport across tens of microns![10] Is this just a curious phenomenon? Apparently not. Intercellular transport-by-nanotube has been likely occurring billions of years between highly divergent species of bacteria.[11] Plus, after tunneling nanotubes’ discovery, it was soon learned that such passages do transport mitochondria, and that this transfer can rescue aerobic respiration in the recipient cells.[12] Although such mitochondrial transport was observed early-on in human mesenchymal stromal/stem cells (hMSCs) and later in many other cell types, it appears that MSCs are uniquely proficient at it; this specialized activity is part of physiologic homeostasis and normal tissue maintenance throughout lifespan.[13] In concert with heath and homeostasis, mitochondria transfer can be stimulated in zones of transient stress like hypoxia gradients and inflammation.
MSCs can also package functional mitochondrial activities and/or physical components into microvesicles (i.e., extracellular vesicles, EVs) and likewise augment the bioenergetics of recipient macrophages.[14] In addition, MSC-to-macrophage transfer appears to involve “outsourcing” of mitophagy—where MSCs eliminate their de-polarized mitochondria by transfer to a nearby “professional waste management” cell type that can “digest” them; this way, MSCs maintain their vitality and only replenish mitochondria with undamaged genomes. A wide body of peer-reviewed literature on the diverse roles of MSC’s “mito-philanthropy” has been accumulating since the mid-2000s. Some of it is expertly reviewed in Amari and Germain (2021),[15] Pers et al (2021),[16] and Liu et al (2021).[17]
The Future of MSC “MitoTherapy” Begins Now
It‘s been convincingly argued that the words to abbreviate “MSCs” ought to be reclaimed as “Medicinal Signaling Cells.[18, 19] Although MSCs vary in tissue of origin and in some complex sets of identity markers, these cells all share basic “auto-medicinal” features. The body stores them in a less-differentiated state—in proximity to vascular tissues—wherein they sense, migrate towards, respond to, and help repair damage in sites of hypoxia, inflammation, infection, ionizing radiation, senescence, or aberrant cell death. Used in over 1000 clinical trials to date, we’re only beginning to grasp their precise mechanisms of action, however. Some bioactivities depend on what the MSCs secrete in a paracrine fashion, such as growth or survival factors, or extracellular vesicles (EVs) and exosomes. Some are dependent on cell-cell contact. And some effects might be dependent on what the MSCs become, e.g., differentiated into bone and cartilage—or “swallowed” by macrophages—which subsequently recruit additional cells to regulate their own specialized tissue repair tasks. In every single one of these physiologic events, mitochondria donation from MSCs might play a decisive role in the choreography of tissue repair. The question naturally arises: can mitochondria from hMSCs be turned into a “medicine?” Basic and/or preclinical investigators are asking this question too. In a very recent exemplar (O’Brien et al, 2021),[20] patients from the SENECA trial (“Stem Cell Injection in Cancer Survivors”)[21] donated peripheral blood mononuclear cells (PBMCs) for reprogramming into iPSCs, and then cardiomyocytes (iCMs). It was then discovered that trial-specific MSCs could secrete mitochondrial activities via larger-sized EVs, which hence provided in vitro protection against doxorubicin-induced injury to the iCMs. Whether or not these unique, ~350nm-diameter vesicles contain actual full-size organelles (which tend to be larger) is probably a matter of further investigation. Nevertheless, these authors justifiably proposed:
“Future studies should determine whether EV-mediated mitochondrial transfer can mitigate AIC [Anthracycline-Induced Cardiomyopathy] in vivo. Further testing in chronic in vivo models of AIC would be valuable because chronic cardiomyopathy models hold greater translational value to humans. In-depth analysis of cardiovascular performance could prove illuminating because rejuvenation of cellular function may prove physiologically significant despite an absence of myocardial regeneration or improvement in ejection fraction.”
Is mitochondrial transfer the next frontier for regenerative medicine? First, we’ve repurposed biology for allogeneic cell and organ transplants, and now behold, organelle transplants? Today, we and others are learning to efficiently harvest quality-controlled[22] EV material from mass-produced MSCs,[23, 24, 25, 26] and the very first clinical trials from these efforts are now underway.[27, 28, 29, 30, 31] Yet, to achieve reliable, scalable, and manufacturable “MSC-mito” materials as IND-ready drug products, cognate drug processes will likewise need robust development efforts. Given the wide span of pathology where there’s observed cascading damage to cellular bioenergetics via conditions like inherited mitochondrial diseases, heart failure, neurodegeneration, diabetes, and aging, surely an unmet need is waiting to be met by this new field’s pioneers.
Perhaps a lesson from the Precambrian needs revisiting? Like the ancient purple bacteria and archaebacteria, multiple scientific, medical, and biotech disciplines might need to engage in a little bit of “symbiosis.” The benefits to kickstart this endeavor will surely be energizing, not merely for regenerative medicine, but most of all, for patients in need.
References
- Sagan, L., On the origin of mitosing cells. J Theor Biol, 1967. 14(3): p. 255-74. 10.1016/0022-5193(67)90079-3
- Muchmore, S. W., et al., X-ray and NMR structure of human Bcl-xL, an inhibitor of programmed cell death. Nature, 1996. 381(6580): p. 335-41. 10.1038/381335a0
- Schirrmeister, B. E., et al., Evolution of multicellularity coincided with increased diversification of cyanobacteria and the Great Oxidation Event. Proc Natl Acad Sci U S A, 2013. 110(5): p. 1791-6. 10.1073/pnas.1209927110
- Lin, S. J., et al., Calorie restriction extends Saccharomyces cerevisiae lifespan by increasing respiration. Nature, 2002. 418(6895): p. 344-8. 10.1038/nature00829
- Gottlieb, E., S. M. Armour, and C. B. Thompson, Mitochondrial respiratory control is lost during growth factor deprivation. Proc Natl Acad Sci U S A, 2002. 99(20): p. 12801-6. 10.1073/pnas.202477599
- Vander Heiden, M. G. and C. B. Thompson, Bcl-2 proteins: regulators of apoptosis or of mitochondrial homeostasis? Nat Cell Biol, 1999. 1(8): p. E209-16. 10.1038/70237
- Wei, M. C., et al., Proapoptotic BAX and BAK: a requisite gateway to mitochondrial dysfunction and death. Science, 2001. 292(5517): p. 727-30. 10.1126/science.1059108
- Cohen, H. Y., et al., Calorie restriction promotes mammalian cell survival by inducing the SIRT1 deacetylase. Science, 2004. 305(5682): p. 390-2. 10.1126/science.1099196
- Caicedo, A., et al., The diversity and coexistence of extracellular mitochondria in circulation: A friend or foe of the immune system. Mitochondrion, 2021. 58: p. 270-284. 10.1016/j.mito.2021.02.014
- Rustom, A., et al., Nanotubular highways for intercellular organelle transport. Science, 2004. 303(5660): p. 1007-10. 10.1126/science.1093133
- Dubey, G. P. and S. Ben-Yehuda, Intercellular nanotubes mediate bacterial communication. Cell, 2011. 144(4): p. 590-600. 10.1016/j.cell.2011.01.015
- Spees, J. L., et al., Mitochondrial transfer between cells can rescue aerobic respiration. Proc Natl Acad Sci U S A, 2006. 103(5): p. 1283-8. 10.1073/pnas.0510511103
- Vignais, M. L., et al., Cell Connections by Tunneling Nanotubes: Effects of Mitochondrial Trafficking on Target Cell Metabolism, Homeostasis, and Response to Therapy. Stem Cells Int, 2017. 2017: p. 6917941. 10.1155/2017/6917941
- Phinney, D. G., et al., Mesenchymal stem cells use extracellular vesicles to outsource mitophagy and shuttle microRNAs. Nat Commun, 2015. 6: p. 8472. 10.1038/ncomms9472
- Amari, L. and M. Germain, Mitochondrial Extracellular Vesicles – Origins and Roles. Front Mol Neurosci, 2021. 14: p. 767219. 10.3389/fnmol.2021.767219
- Pers, Y. M., C. Jorgensen, and M. Khoury, Editorial: The Role of Metabolism in MSC-Mediated Immunomodulation. Front Immunol, 2021. 12: p. 751865. 10.3389/fimmu.2021.751865
- Liu, D., et al., Intercellular mitochondrial transfer as a means of tissue revitalization. Signal Transduct Target Ther, 2021. 6(1): p. 65. 10.1038/s41392-020-00440-z
- Caplan, A. I., There Is No “Stem Cell Mess”. Tissue Eng Part B Rev, 2019. 25(4): p. 291-293. 10.1089/ten.TEB.2019.0049
- Rodriguez-Fuentes, D. E., et al., Mesenchymal Stem Cells Current Clinical Applications: A Systematic Review. Arch Med Res, 2021. 52(1): p. 93-101. 10.1016/j.arcmed.2020.08.006
- O’Brien, C. G., et al., Mitochondria-Rich Extracellular Vesicles Rescue Patient-Specific Cardiomyocytes From Doxorubicin Injury: Insights Into the SENECA Trial. JACC CardioOncol, 2021. 3(3): p. 428-440. 10.1016/j.jaccao.2021.05.006
- The University of Texas Health Science Center, Houston, Lung National Heart, and Institute Blood, Stem Cell Injection in Cancer Survivors. 2019.
- Thery, C., et al., Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J Extracell Vesicles, 2018. 7(1): p. 1535750. 10.1080/20013078.2018.1535750
- Yeo, R. W., et al., Mesenchymal stem cell: an efficient mass producer of exosomes for drug delivery. Adv Drug Deliv Rev, 2013. 65(3): p. 336-41. 10.1016/j.addr.2012.07.001
- Katrina Adlerz, Michelle Trempel, Jamie Brennan, Jon Rowley, Taby Ahsan. MSC-EVs Manufactured in Scalable 3D Bioreactor Systems. 2019; Available from: https://www.roosterbio.com/wp-content/uploads/2019/10/2019-BPI-EV.pdf.
- Adlerz, K., et al., Strategies for scalable manufacturing and translation of MSC-derived extracellular vesicles. Stem Cell Res, 2020. 48: p. 101978. 10.1016/j.scr.2020.101978
- Rowley, Jon. Radically Simplifying Production of hMSC-EVs with Rapid Clinical Translation & Scale-up Potential. RoosterBio Webinar 2020; Available from: https://bit.ly/3AqZOQm.
- Carson, Jonathan. It’s Not Rocket Science – “MSC-EVs” Have the Right Stuff. 2021; Available from: https://bit.ly/3B7Byn8.
- Kalluri, R. and V. S. LeBleu, The biology, function, and biomedical applications of exosomes. Science, 2020. 367(6478). 10.1126/science.aau6977
- Wiklander, O. P. B., et al., Advances in therapeutic applications of extracellular vesicles. Sci Transl Med, 2019. 11(492). 10.1126/scitranslmed.aav8521
- Adlerz, Katrina and Patel, Divya. MSC-EVs Emerge as Clinical Therapies 2020; Available from: https://www.roosterbio.com/blog/msc-evs-emerge-as-clinical-therapies/.
- Lenzini, Stephen. Big Effects in Small Packages: What Are Extracellular Vesicles, Exosomes, & Microvesicles & Why Are They En Route to the Clinic? RoosterBio Blog 2021; Available from: https://www.roosterbio.com/blog/big-effects-in-small-packages-what-are-extracellular-vesicles-exosomes-microvesicles-why-are-they-en-route-to-the-clinic/.
