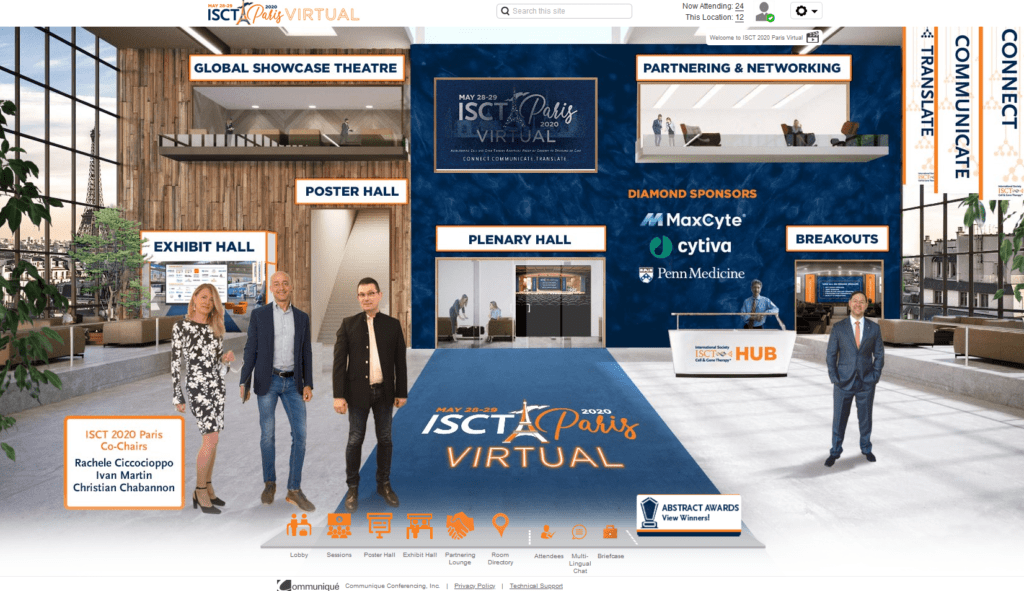
This year’s ISCT conference had a different look than in years past, as the organizers quickly pivoted from planning a conference in Paris to a fully virtual event due to the COVID-19 pandemic. The virtual event impressively had all of the usual elements with live sessions, a poster hall, exhibit hall, and networking room all packed into an exciting two days, taking place between 8:00 a.m. EDT Thursday May 28 and 8:30 p.m. EDT Friday May 29, with pre-recorded sessions available for viewing over the next year.
More importantly than the change in venue, the conference adjusted to a new focus on how to treat patients both currently suffering from COVID-19 as well as future patients of the pandemic, in addition to the typical updates from the Cell & Gene Therapy field.
Below are just a few of the key takeaways from the content-packed conference about the current state of Cell & Gene Therapy and COVID-19’s potential to impact the field.
COVID-19 has the potential to dramatically affect the cell therapy field.
Along with the rest of the medical industry, the Cell & Gene Therapy field rapidly mobilized to offer potential treatments for patients suffering from COVID-19. In fact, as highlighted in the Opening Plenary session by Dr. Dan Weiss, there are currently ~70 registered cell therapy clinical trials expected to treat >3,500 COVID-19 patients, with MSCs as the leading cell source due to their immunomodulatory capabilities (previously discussed in RoosterBio blogs on Covid-19 and ARDS). This quick mobilization is due in part to companies such as Athersys. Dr. Anthony Ting explained how Athersys, whose cell therapy to treat ARDS recently received Fast Track designation by the FDA, worked quickly to expand their phase II/III trial to also include ARDS in COVID-19 patients. Similarly, Dr. Rita Barcia of Sentien Biotechnologies explained how their extracorporeal MSC device, currently in clinical trials to treat kidney injury, might have promise for COVID-19 patients based on the similar cytokine profiles observed in the kidney injury patients and COVID-19 patients. In addition to industry-led clinical trials, many studies are also being supported by academic institutions. Dr. Patricia Rocco discussed multiple clinical trials, including those investigating varying doses and others that compare Bone Marrow-derived to Umbilical Cord-derived MSCs, as well as EVs.
There are currently limited results available from these clinical trials as the COVID-19 crisis emerged just in the last 6 months, but there is hope that these treatments will ultimately help patients. It was stressed, however, by all speakers including Dr. Maroun Khoury (first author of the Cytotherapy article on this subject) that this is also a pivotal moment for the Cell Therapy field. Properly designed clinical trials with fully transparent methodology are critical in order to accurately assess the impact and promise of these cell therapy treatments. There was significant discussion about appropriate testing and endpoints and the importance of randomized trials. If these treatments show promise, we might be entering, as Mr. David Smith called it, a “Golden Age of Cell & Gene Therapy” where cell therapy treatments develop more rapidly and become available to treat patients.
Regulatory agencies have shown to be adaptable.
As mentioned, the number of clinical trials for COVID-19 increased very quickly. This is due to industry and academia realization of the unmet need, and of robust compelling preclinical data with cell therapies. Also, the regulatory agencies typically now give feedback at an extremely accelerated pace (previously discussed here). There was a sense of tangible hope from those involved in these clinical trials that some of this rapid feedback and decision-making might proceed through future clinical trials, and accelerate future therapies’ progressions into larger scale manufacturing for patients.
Dr. Laura Niklason, co-founder of Humacyte, discussed working with regulators for a tissue engineering product, an even less well-established field than cell therapy in terms of clinical trials. She discussed how the regulators were adaptable when presented with the right data. These “right data” have advanced Humacyte’s human acellular vessel product from initially being uncategorizable by regulatory agencies to now entering into a Phase III clinical trial, with hopes for commercialization.
Scalable manufacturing will be a focus of the field moving forward.
Considering the prospect of ultimately successful Cell & Gene Therapy in the treatment of COVID-19 and/or other diseases–and regulatory pathway acceleration–it was discussed that the field needs to do some work to be prepared for the coming “Industrialization”. An entire conference tract was devoted to this theme which included discussions around the importance of having a plan for scalable manufacturing when starting early phase clinical trials as well as a few other ideas.
For example, while the approved CAR-T cell therapies are based on the autologous approach, there is discussion about whether allogeneic cells might offer a better manufacturing paradigm with ongoing work to confront the technical and biological hurdles. iPSCs were also offered by Lonza’s Alberto Santagostino as another future alternative cell source given their inherent scalability.
There are still technical details to be worked out on the manufacturing side and the clinical administration of cell & gene therapies. Strategies to address donor-to-donor variability of the cells is one such challenge. Dr. Halvard Bonig presented his team’s approach to neutralizing donor-to-donor variability: a cell product was produced from pooling mononuclear cells from many donors, and then expanding the cells to working cell banks as one batch. This product has been used to treat GVHD patients in Europe under a pharmacovigilance study. Clinical administration of cell therapies may also need to be optimized to balance potency and ease of administration. Dr. Jacques Galipeau called for investigating the effects of cell therapies that are directly administered after cell thaw compared to therapies administered after a short post-thaw culture rescue.
The cost of goods of cell & gene therapies is another challenge to industrialization with critical raw materials, scale, and manufacturing platform all critical considerations. RoosterBio’s Dr. Josephine Lembong presented a poster on manufacturing bone marrow-derived MSCs with a bioreactor platform, detailing the development, optimization, and scale-up of a xeno-free fed-batch bioreactor process with data up to the 50L production scale. A similar poster was presented showing the bioreactor system and scale-up with human umbilical cord-derived MSCs.
Automation was another common strategy proposed to move the field towards industrialization. For example, automation was discussed by Dr. Emanuele Ostuni of Novartis Europe, who has worked on Novartis’ autologous CAR-T product, Kymriah. Dr. Niklason, in turn, discussed Humacyte’s automation strategy. Dr. Niklason pointed out that the cost to automate a step performed once during the manufacturing process will likely yield less efficiency and may not be worth the cost, instead calling for the focus to be on the automation of repeated steps.
Genetic engineered cells have additional challenges in scalable manufacturing, and accordingly Dr. Philip Lee of Senti Biosciences presented a manufacturing scheme for Genetic-Engineered cells as Senti advances to GMP manufacturing. He showed that starting with human bone marrow-derived master cell banks, they are able to scalably manufacture a genetically engineered cell product, with a single bone marrow collection able to produce >80,000 final product doses.
Like tissue engineering, the EV field seems to be in a similar trailblazing era. With very few clinical trials to draw precedent from, the field is striving to work together to advance the state of basic knowledge and forge into clinical therapies, given the therapeutic promise of EV therapies. Dr. Sai-Kiang Lim discussed some of the possible mechanisms and benefits of EV treatments, while Dr. Rebecca Lim discussed how EVs may have additional advantages compared to cells. For example, with her work in premature neonatal patients, it was observed that EVs could be more easily administered than cells due to the EVs’ small size. To confront the standardization challenge of industrialization, the EV field is taking multiple approaches, from trying to generate reference material for EVs (an effort led by Dr. Ann Hendrix), to defining what exactly are the most important CQAs for EVs as discussed by Dr. Mario Gimona of Celericon Therapeutics as Celericon is planning to take MSC-EVs into Phase I/II clinical trials for treatment of auditory hair cell decay. Similarly, increased understanding of the effects of manufacturing decisions on EV final products will weigh more heavily on the field as it moves towards industrialization. For instance, EV pioneer Dr. Clotilde Thery presented a matrix to understand and categorize the various downstream EV processes, based on specificity and process recovery. RoosterBio also presented a poster on new product development and scalable manufacturing for MSC-EV generation highlighting process development decisions like manufacturing platform and raw materials that, when considered early in process development, could accelerate the path to the clinic as the field moves towards industrialization.
Future of Cell & Gene Therapy
This year’s conference, despite being virtual, captured the excitement and potential of the Cell & Gene Therapy field, with just a few key themes highlighted above. Next year’s 2021 conference will surely be one not to miss with preliminary results of many of these COVID-19 clinical trials expected and perhaps ushering in the dawn of a new Golden Age of Cell & Gene Therapy.
For Reference
Sentien Biotechnologies’ Pivot to COVID
Humacyte Press Release
